Missouri’s Medicaid program is out of control, and state lawmakers don’t seem to care. Enrollment in the state’s program keeps setting new record highs every month, with more than 1.5 million Missourians now enrolled. But new estimates suggest that more than 20% of enrollees shouldn’t be on Medicaid at all, as they no longer meet the program qualifications.
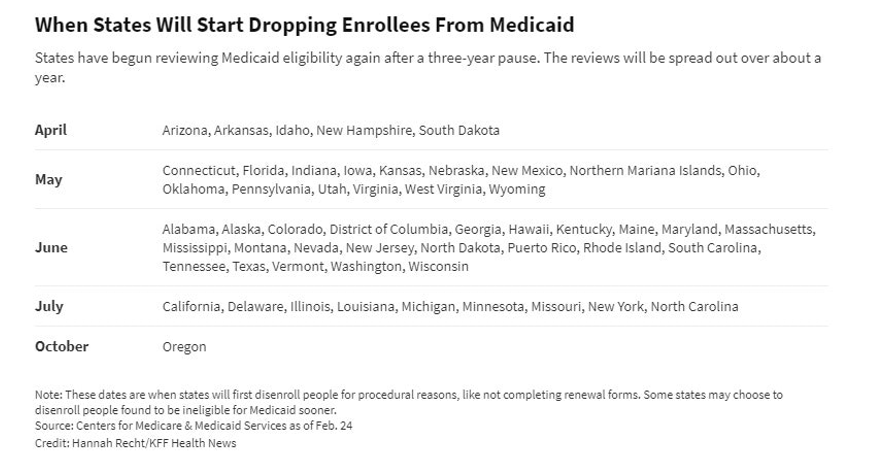
Over the past two months, many states across the country—but not Missouri—have started deflating their bloated Medicaid rolls. (Reminder: enrollment got to be this high because prior to April of this year, the federal government barred states from checking eligibility or removing anyone from the program since March of 2020, as part of the response to COVID-19.)
Unfortunately, the Centers for Medicare and Medicaid Services reports that Missouri is waiting until July before removing any ineligible enrollees. If true, Missouri stands in stark contrast to states such as Florida or Arizona that started checking their Medicaid enrollees’ eligibility as soon as the federal prohibition was lifted. Recent articles suggest that Florida has already identified upwards of 250,000 ineligible enrollees, which translates to significant savings for taxpayers.
In theory, removing ineligible recipients from government-sponsored health coverage shouldn’t be a controversial topic. Prior to COVID-19, states were required by federal law to check whether their Medicaid enrollees were still eligible for the program at least once every year but could check as frequently as every six months.
Regular redeterminations (eligibility checks) are important because people’s circumstances change frequently, and they may not always go out of their way to inform the government of any changes. In Missouri, like many other states, the government pays health plans monthly to provide health coverage to Medicaid recipients, regardless of whether they receive any services. Given how expensive health coverage is, this means that there are likely billions of tax dollars being spent improperly on the program every single month.
With hundreds of thousands of eligibility checks needed, the potential for significant reductions in wasteful government spending is why states are rushing to clean their Medicaid rolls. It’s also why I suggested Missouri consider hiring outside help for processing redeterminations, given how difficult an administrative task it would be.
Though it’s just another thing to add to the list of this year’s legislative failures, it’s telling that our elected officials couldn’t even get out ahead of something as long choreographed as the resumption of Medicaid eligibility checks. If spending is all about priorities, it’s clear Missouri’s elected officials don’t consider reducing government waste to be one of them.